Miscarriage, also known as abortion, is the natural rejection of a pregnancy embryo or fetus before it reaches a viable age. It is important to understand that miscarriages are relatively common, especially early in pregnancy, and they can happen for various reasons. Here are some of the most common causes of miscarriage:
- Genetic abnormalities: Miscarriages are often caused by genetic abnormalities in the embryo that make it non-viable. This may be a natural way the body prevents the birth of a child with serious genetic defects.
- Chromosome abnormalities: Chromosome defects in the embryo can cause it not to develop normally, and this can result in a miscarriage.
- Hormonal problems: Hormonal imbalances, such as low levels of progesterone needed to maintain a pregnancy, can lead to a miscarriage.
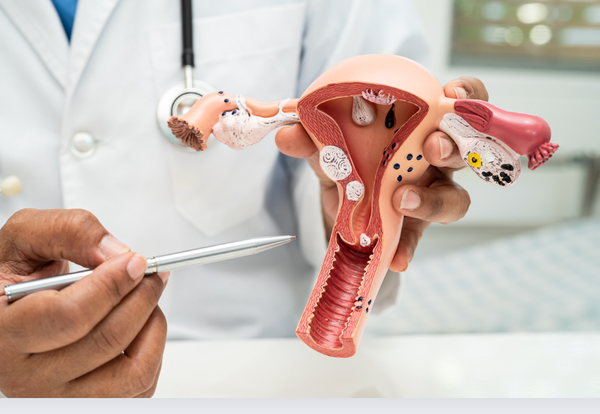
- Anatomical problems: Physical problems with the uterus or fallopian tubes can affect the ability to maintain a pregnancy.
- Age: The woman's age plays a role, as the risk of miscarriage increases with age, especially after the age of 35.
- Infections: Certain infections, such as cytomegalovirus (CMV) or listeriosis, can cause miscarriage if they affect the embryo.
- Autoimmune diseases: Autoimmune diseases can cause the body to attack the embryo as a foreign invader.
- Medicines or drugs: Some drugs or drugs can increase the risk of miscarriage.
- Lifestyle factors: Smoking, excessive alcohol consumption and unhealthy diet can also increase the risk of miscarriage.
- Stress: Severe stress can affect hormone levels and have a negative impact on pregnancy.
It is important to note that in many cases miscarriage is a natural process that cannot be prevented or stopped. Most women who experience a miscarriage can later achieve a healthy pregnancy. However, if you experience recurrent miscarriages, it is important to seek advice from a gynecologist or fertility specialist to rule out any underlying causes and to get advice on how to improve your chances of a successful pregnancy.
Book appontment